Into Oblivion: The Vortex of Addiction
Anyone caught in the vicious cycle of addiction can appreciate the term "vortex" as a description of their experience. Addiction is a chaotic and painful experience that revolves around the destructive use of substances or behaviours. Addiction leaves a trail of carnage in its wake. There is immense damage to physical and mental health, relationships, finances, career prospects, and even one's sense of self. Addiction is a vortex. People who experience the devastating grip of addiction describe being pulled further into something they cannot escape.
Those who struggle with addiction are baffled by their behaviour. But, unfortunately, an honest desire to stop harmful patterns doesn't always lead to lasting change – no matter how strong the desire for change is.
There are many theories about what contributes to substance use and addiction disorders. Genetics, family history, social influences, and mental health can all play a role. There are also moral judgements about those who struggle with addiction: they are lazy, selfish, or just in pursuit of pleasure. But what if there is a way to better understand the behaviours and consequences of addiction? What if there is a more compassionate and supportive way to understand the process of addiction and what helps someone recover?
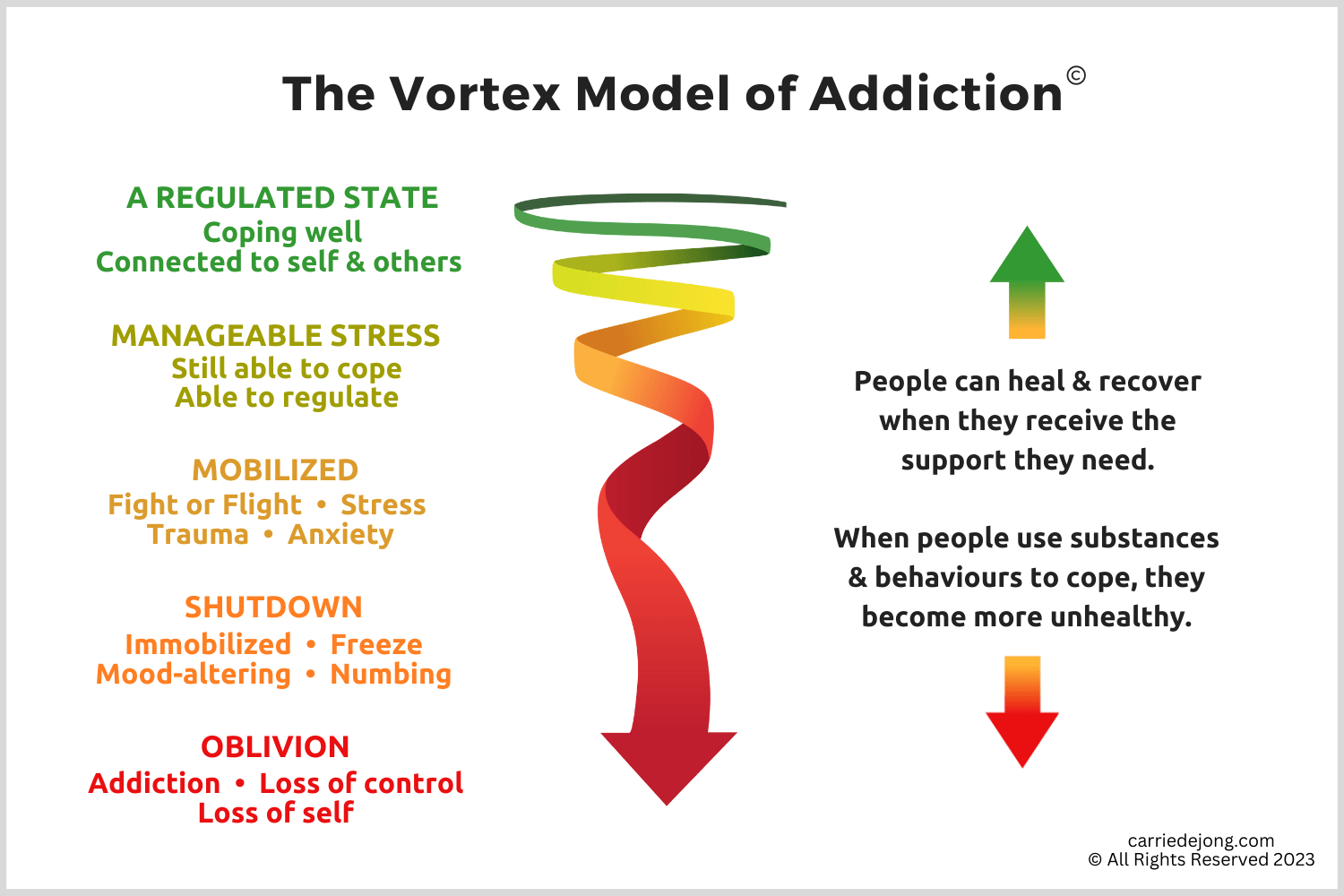
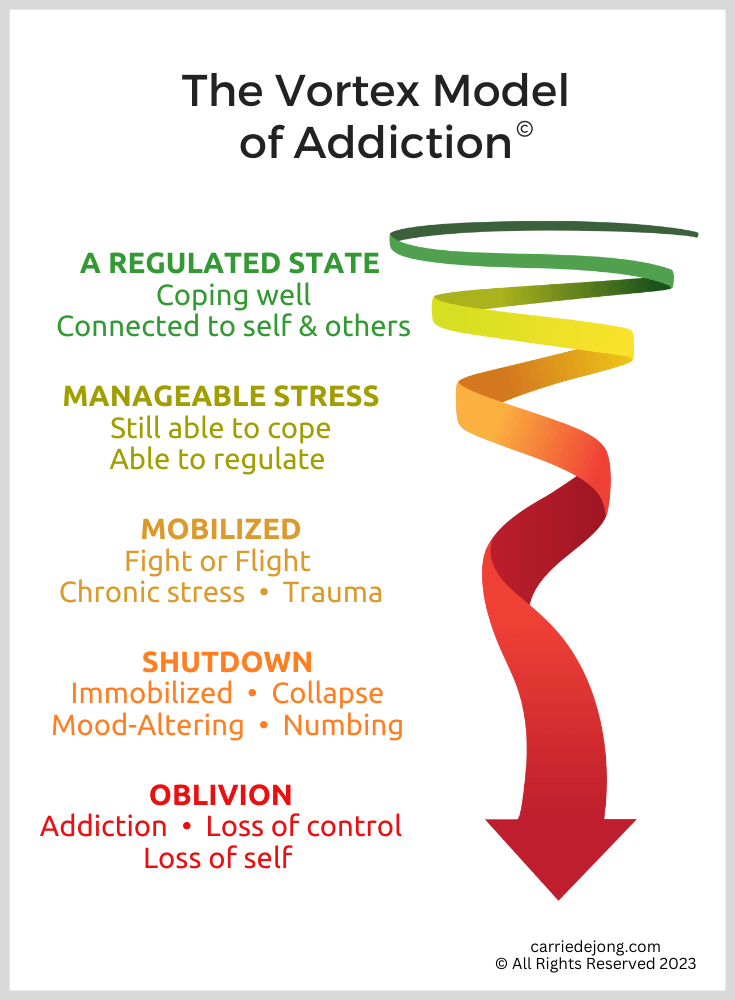
The Vortex Model of Addiction does just that. It demonstrates how circumstances, life events, and responses to overwhelming events contribute to the transition into addiction. It also provides information about how our brains and bodies are wired – invaluable information when addressing substance use and addiction disorders.
Below is a diagram that outlines where we are going. If you are interested in a much shorter version of this information, click here.
LAYING THE GROUNDWORK
I'm excited to share this model of addiction I have developed over my 25 years as a counsellor in this field. Before I explain the model, it’s essential to set the groundwork. The research of other clinicians and scientists has shaped my understanding of addiction. This research includes understanding the link between trauma and addiction. My work as a therapist has also been heavily influenced by growing knowledge of the human brain and nervous system and newer approaches to healing trauma.
The Link Between Trauma and Addiction
Many articles I have written focus on the connection between trauma and addiction. My eBook, Trauma and Addiction: The Link We Can't Ignore, offers an in-depth exploration of this topic. It outlines how traumatic experiences paves the way for using substances and behaviours to self-medicate the common impacts of trauma.
Research shows that someone with PTSD is four times more likely to have a problem with substance misuse than someone without PTSD. (1)
While trauma isn't always a contributing factor, painful life experiences are known to contribute to addiction. The Adverse Childhood Experience (ACE) Study reveals a strong correlation between traumatic childhood experiences and addiction. (2)
These two issues need to be addressed together for anyone with a history of trauma and addiction. If not, it leads to more significant struggles for both problems.
Substance use often starts as a way of managing trauma's overwhelming symptoms, including anxiety, shame, uncomfortable physical sensation, and intrusive thoughts.
Ongoing Neuroscience and Trauma Research
The Vortex Model of Addiction draws from the work of many well-known researchers in trauma and neuroscience. Over the past two decades, scientists have provided profound information about how our brain and nervous system are wired. Some of the research that strongly influences my understanding of trauma and addiction include:
The Adverse Childhood Experiences Study by Dr. Felitti and Dr. Anda demonstrates the strong link between childhood trauma and the development of addiction. (2)
Somatic approaches to trauma therapy, such as the work of Peter Levine’s “Waking the Tiger” (3) and Bessel van der Kolk’s “The Body Keeps the Score”. (4)
Stephen Porges' Polyvagal Theory, a complex theory about the human nervous system and our biological responses to safety and danger. (5)
The "Window of Tolerance" introduced by Daniel J. Siegal. (6)
UNDERSTANDING OUR NERVOUS SYSTEM
The Vortex Model of Addiction is built on understanding how our nervous system responds to stressful and traumatic experiences. The human nervous system is our primary operating system – our body’s command center. Yet, too often, we know very little about what this system does, how it functions, or what happens when we encounter challenges.
Our nervous system is responsible for various tasks: thoughts, emotions, memory, sensation, behaviours, reactions, movement, bodily functions, and instincts.
Understanding our nervous system helps us understand ourselves better. This is especially true of the value of learning about the autonomic nervous system (ANS), one of the major divisions of our nervous system. The ANS is responsible our involuntary bodily processes like digestion, temperature regulation, and heart rate. It also manages our instinctive reactions when we encounter any threat.
Although much of our ANS operates in predictable ways, most functions occur outside our conscious awareness. We don’t have to think about digesting lunch. Our body regulates its temperature without us needing to do anything. In the same way, our ANS automatically responds to dangers or threats without involving our thinking brain. When we touch something hot, our ANS responds, and we instinctively pull our hand back long before our thinking brain realizes what happened.
The ANS is also involved in our response to trauma and stressful life events.
Understanding our biology is crucial to making sense of the impacts of stress and trauma. Understanding our biology also helps make sense of the move into unhealthy patterns of substance use or other addictive behaviours as a coping mechanism. This is especially true when our nervous system is exposed to trauma or chronic stressors. These tax our system making it more difficult to regulate in healthy ways.
Adverse life events challenge our ability to maintain physical, emotional, mental, and relational health.
When we experience adverse life events, it dysregulates our nervous system. As a result, regulating our bodies, emotions, behaviours, thoughts, and relational capacities becomes much more challenging. Trauma sets the stage for using substances or behaviours as a way to cope.
THE VORTEX MODEL OF ADDICTION
So far, I have provided some basic information about our nervous system. This information is foundational to understanding the Vortex Model of Addiction. Next, I outline five categories our nervous system can experience - they generally follow the states outlined in Stephen Porges' Polyvagal Theory (5).
The Vortex Model of Addiction provides a way of understanding the move into addictive patterns with substances or behaviours. It speaks to the progressive nature of substance use and addiction disorders. Those who struggle can attest to how addiction's impacts grow over time. But this model also speaks to the progressive nature of trauma symptoms. Lastly, the Vortex Model also speaks to the process of recovery.
A Regulated State
We function best when most aspects of our lives are manageable. We are healthiest when our nervous system is regulated – when we can cope with stressors but still experience periods of calm and restoration. A regulated state includes our ability to:
Take good care of our physical bodies
Enjoy healthy and supportive relationships
Regulate our emotions and our reactions
Demonstrate good judgment and clear thinking
Regulate our behaviours and choices
Cope well with everyday challenges
Individuals who find it easy to experience a regulated state actively address issues in their lives. They typically take good care of themselves. They participate in supportive relationships and meaningful social, academic, or vocational endeavours. They tend to possess a healthy repertoire of coping skills and are good at reaching out for support when needed.
Most people who misuse substances or engage in mood-altering behaviours as a coping method tend to find it challenging to consistently engage in life and relationships in these healthy ways.
Those who experience addiction disorders rarely enjoy a true sense of calm.
Manageable Stress
We all know life does not remain calm. Our modern lives are far too complicated for that. There are numerous sources of stress: deadlines, traffic delays, minor illnesses, or a quarrel with a loved one. In addition, daily situations can place higher demands on our self-regulatory processes. Frustration, work pressure, excitement, and performance require more physical, emotional, or cognitive energy.
It's important to note that not all of this increased stress is negative. For example, delivering a speech or falling in love increases the demands on our nervous system but are not necessarily unwanted or unpleasant experiences.
People who are well-regulated find ways of engaging in more challenging or taxing activities but are not overwhelmed by these demands.
At the end of a stressful situation, they can decompress and find a way back to a calm and regulated state. Perhaps a good meal, connection with a loved one, exercise, or a good sleep helps "reset" their nervous system enabling them to return to a state of calm and manageability. In addition, their nervous system is flexible enough to allow them to move in and out of more challenging situations relatively easily.
But life doesn’t stay manageable. This is where the journey to addiction begins.
The following three categories (Mobilized, Shutdown, and Oblivion) become more problematic for those who struggle with substance use and addiction disorders. Patterns of harmful substance use and mood-altering behaviours begin to take root in these two stages when people self-medicate trauma symptoms, anxiety, or chronic stress.
Mobilized
If only life remained manageable – but it clearly doesn't. How many times a day do we hear words like "stressed out" or "exhausted"? Everything feels hurried and stressful. We don't need to look very hard to see how we have ramped up our lives over the last few years. We have non-stop social media feeds, 24-hour news channels, and energy drinks.
While some would argue that busyness is a sign of progress, it actually taxes our ability to cope. It takes a toll on all of us. Our health, mental health, and relationships show signs of pushing ourselves too hard. Anxiety-related challenges have risen dramatically. Workplace absenteeism due to mental health concerns is skyrocketing. There are resources and suggestions for managing stress or anxiety everywhere we look.
A mobilized state occurs when our sympathetic nervous system (SNS) is activated.
The SNS is the branch of the autonomic nervous system (ANS) responsible for mobilization and our fight or flight response. Polyvagal Theory describes this state of mobilization extensively. (5). When our body initiates a stress response, many things occur. For example, cortisol and adrenaline are released. Our heart rate and blood pressure increase. Our nervous system automatically initiates these changes to help fight or flee the threat we are facing.
This sympathetic nervous system activation makes sense when a bear is chasing us or we need to respond quickly to some threat. However, it is more challenging for our nervous system when the threat is chronic and ongoing – like anxiety or stress.
Ideally, our nervous system then shifts us back into a more manageable state of activation by engaging the parasympathetic branch (the rest and digest branch) of the nervous system. But unfortunately for many, this shift back into a regulated state may not happen easily or often enough.
Anyone who experiences chronic stress or anxiety is living in a chronically mobilized state. Many of the experiences that fall into the mobilized state in the Vortex Model are the recognizable symptoms of high anxiety or chronic stress that include:
Excessive worry
Overthinking
Rapid heartbeat
Gastro-intestinal issues
Irritability
Decreased social connection
Busyness
Insomnia
Overwhelming emotions and emotional reactions
Trauma and the Impacts of Trauma
Besides the common experiences of increased stress or anxiety, trauma also produces a highly mobilized state. As I have previously discussed, many of those who experience addiction have also been impacted by trauma. Accidents, illness, violence, abuse, neglect, natural disasters, and other traumas are common among those struggling with substance use and addiction disorders. We know these experiences trigger a "fight or flight" response during the traumatic event. But this state doesn't always resolve once the trauma is over.
While healing can occur following a trauma, many exposed to adverse life experiences have not had the support to heal. This means their nervous system remains impacted by their traumatic experiences.
For those who have unresolved or unhealed trauma, the mobilized state is the high level of activation that remains in the nervous system and the physical body following a traumatic experience. It is an ongoing fight or flight response activation even after the threat or trauma has ended. A person who has experienced a trauma may continue to experience high nervous system activation that alters their experience of self, the world, and others. These disruptions can, unfortunately, continue for years or decades.
Trauma researchers divide the impacts of trauma into two groups. The first category is “hyper-arousal”, referring to too much activation or energy in the nervous system. The second category is “hypo-arousal” – when the nervous system responds to trauma by numbing and shutting down. There will be more about this category later. My eBook provides more information about these two types of trauma symptoms.
The mobilized state also includes many of the common impacts of trauma, especially those in the “hyper-arousal” category:
Your nervous system remains on high alert: You might be more jittery or startle easily. You might be more emotionally reactive. And experience more irritability, aggressiveness, or impulsivity. Perhaps you are hypervigilant – always watchful for any sign of a potential threat. Insomnia can also be a common problem if our nervous system continually scans for possible danger.
Physical Symptoms: When our nervous system remains on "high alert", our body also remains on high alert. Symptoms of this can include tension, digestive problems, excessive sweating, and elevated heart rate. These overwhelming physical sensations can continue following a trauma resulting from the fight or flight response remaining activated long after the danger has passed.
Mental Symptoms: “A "busy brain", difficulty concentrating, obsessive or irrational thoughts, and overthinking are everyday experiences for those who are mobilized. There can also be challenges with learning or practicing self-control.
Emotional Reactivity: A mobilized state contributes to difficulties with regulating strong emotions. It also makes it more likely a person will see harm where none was intended. Or they may become defensive when challenged or criticized. For those who have experienced trauma, the ongoing experience can be one of reliving the primary emotions of trauma, including heightened anxiety, fear, or shame. There can also be a more significant struggle with expressing anger appropriately.
Re-experiencing Symptoms: For those who have experienced trauma, these profoundly disturbing experiences include trauma-based flashbacks, nightmares, and intrusive images. Intrusive experiences are the ways you may continue to relive your original trauma.
Unhealthy Behaviours: For individuals who spend a good portion of their life in a mobilized state, unhealthy behaviours are often an attempt to “manage” the overwhelming experience of hyper-arousal. Self-harm, disordered eating, compulsive sexual activity, and problematic substance use are much more common among people with traumatic experiences.
Trauma and other painful events move our nervous system past its ability to regulate itself. While anxiety, stress, and traumatic experiences are common to the human condition, the good news is that we can recover from these challenges. To heal, we must receive the support and help we need. When this happens, many of these symptoms can resolve over time – allowing us to return to a more regulated state. With adequate support, we can move back into a state of greater coping. However, for some, therapy involves a longer process of developing tools and resources that support a move into greater emotional, relational, and mental health. Unfortunately, not everyone receives the support they need to heal.
Some people have experienced more trauma than their nervous system can cope with. This is what sets people up for substance use and addiction disorders.
Mood-Altering in the “Mobilized” State
Being stuck in a fight or flight response is exhausting, distressing, and painful. So understandably, people who live in a highly mobilized state will seek ways to give themselves a break if they don't easily return to a regulated state.
What happens when people don't have the tools or resources to cope with anxiety, chronic stress, or trauma? They start to self-medicate.
Those who experience the symptoms of stress or anxiety often mood-alter. People with addiction are often medicating their trauma symptoms.
One of the ways people "take the edge off" is to do something that keeps them in a mobilized state but acts as a way to "check out" or "numb". For example, they may use substances or behaviours that keep the nervous system in sympathetic nervous system activation. The person's state doesn't change – it's still mobilized. But they are just giving themselves a different experience of mobilization that numbs or gives them a break from the discomfort they otherwise experience.
Here are some examples of mood-altering in a mobilized state:
Excess caffeine use
Stimulant drug use (cocaine, methamphetamines)
Compulsive exercise
Gaming
Gambling
Compulsive Spending or Shopping
Compulsive sexual behaviours
High-risk activities
The second way people take the edge off being mobilized is to disconnect from themselves, others, and the world around them. This brings us to the next stage of the Vortex of Addiction: Shutdown.
Shutdown
We name it in many ways: numb, numbed out, checked out, disconnected, shutdown. Then think about the phrases that describe some of the ways people numb out: "drowning our sorrows", "taking the edge off", and "feeling no pain". While there are many different descriptions, they all point to the desire or need to disconnect from uncomfortable or painful things.
Disconnecting and shutting down obviously feels better – that's why it is a common response to the exhausting experience of chronic mobilization.
Understandably, some want to feel "nothing" rather than feeling "everything". This is especially true when dealing with the unrelenting painful thoughts, feelings, or sensations associated with anxiety, chronic stress, or trauma.
People who have experienced trauma can have entirely different symptoms than those in the mobilized or hyper-arousal category. Instead, they may experience hypo-arousal symptoms. Rather than a state of high activation, hypo-arousal shows up as a state of "shutdown" that results when trauma and traumatic stress become overwhelming. As a result, the nervous system moves into dissociative and disconnected responses.
Hypo-arousal is a state of disconnection, and the result is that we feel or experience “too little”.
Our nervous system can shut down when trauma and chronic stress become overwhelming. “Dissociation” is one of the clinical words often used to describe this state of shutdown. If the hyper-arousal state is the “fight or flight” response, then the hypo-arousal state is the “freeze” response. Polyvagal Theory refers to this state as Immobilization. (5)
A wide variety of experiences occur in this shutdown stage. Clinical symptoms can include depression or dissociation (feeling disconnected from self, others, and the world around you). Other common experiences of shutdown include:
Emotional Numbness: There can be a sense of detachment or emotional emptiness. People may be out of touch with their emotions to protect against painful feelings. They may have difficulty feeling or identifying emotions. For some, this numbness happens automatically. For others, substances or behaviours help create emotional numbness.
Painful Emotions: Those who experience emotion may feel overwhelmed or helpless. Some may experience profound hopelessness or despair. While shame can initially be a highly mobilized state, chronic shame can become an emotion that shuts people down.
Relational Avoidance and Isolation: Traumatic experiences can create a tendency to withdraw and isolate. Unresolved trauma, primarily relational trauma, can make someone more comfortable avoiding intimacy or connection with other people.
Physical Symptoms: The "too little" symptoms that impact the body include having little or no energy to complete daily tasks. The experience of fatigue or exhaustion is common. In addition, trauma can affect the ability to feel sensations in the body.
Cognitive Symptoms: Some people may have challenges thinking clearly. They may be forgetful or “spaced out”. It can also be common to have memory challenges.
Behavioural Symptoms: It can be common to feel overwhelmed and unable to cope with essential parts of life.
This experience of shutdown or disconnection helps make a painful experience more tolerable in some ways. Trauma researcher Peter Levine says that dissociation “helps make unbearable bearable.” (3) This reaction occurs without conscious thought – an automatic response to an overwhelming experience. And it happens, in part, as a way of protecting us from the painful experience of trauma symptoms. So what happens to those who are not able to heal and recover?
The answer is simple: they shut down to disconnect from the pain.
For some people, the capacity to shut down or dissociate occurs more easily. This tends to be true for those exposed to significant trauma as children – they learned to cope with overwhelming pain by shutting it off. Research tells us that if dissociating was a coping tool as a child, it often remains a powerful coping tool in adult life. For others, the ability to disconnect from painful experience of trauma doesn't happen easily or naturally – unless there's a little help from substances or behaviours. This is another of the reasons people mood-alter.
Mood-Altering in a Shutdown State
As discussed earlier, there are generally two different goals people have when they mood-alter in a mobilized state:
To offer a numbing experience that still keeps them mobilized.
To move them from a mobilized state to shutdown. If someone experiences chronic anxiety or past trauma, mood-altering helps numb this painful experience.
Dr. Willie Langeland and her colleagues point out that some people with a history of trauma and addiction disorders may experience less trauma-related dissociation. So they likely rely on mood-altering substances (or behaviours) to help them. (7) Remember trauma researcher Peter Levine's statement about dissociation: "It helps make the unbearable bearable."
Mood-altering substances and behaviours may attempt to soothe or numb the painful symptoms of trauma and chronic stress. They may be a way to shut down the pain they feel.
There are also two reasons people mood-alter when they are already experiencing a state of shutdown:
To help themselves stay numb.
To move them into a mobilized state – some people mood-alter to feel something other than a chronically numb state.
It makes sense that those who spend significant time in a state of shutdown and immobilization may want to mood-alter to make their life more bearable in that state. Understandably, some want to feel “nothing” rather than feeling “everything”. This is especially true when dealing with the unrelenting painful thoughts, feelings, or memories associated with anxiety, chronic stress, or trauma.
So some may choose to numb even more by using opiates, cannabis, or alcohol to soothe their painful experience.
But those who live in a constant state of numbness and detachment may be more drawn to high-risk behaviours instead. They may experience an increased desire to engage in risky behaviours or sensation-seeking in dramatic ways, including high-risk substances. Behavioural addictions such as sex or gambling addiction are another way. Someone may want to feel something rather than nothing.
Whatever the goal of using is, it’s creating a destructive pattern that pulls someone deeper down the vortex of addiction.
The Consequences of the Shutdown State
Although this state of shutdown and hypo-arousal can "feel better" than being mobilized, it is certainly not healthier. On the contrary, it only brings increased damage that results from an ongoing disconnection from more beneficial resources, coping tools, and relationships. The further down the Vortex of Addiction a person travels, the less likely they are participating in activities and experiences that occur in a regulated state.
Rather than the benefits coming from a regulated state, those who are consistently shutdown in their addiction are struggling:
They experience poorer health and mental health
Their relationships are often strained
They have difficulty regulating their emotions and actions
The ability to think clearly and make sound judgments are severely impacted
There is an inability to cope with everyday challenges
It isn’t difficult to see what happens when people try to disconnect from the overwhelming and painful symptoms of unresolved trauma with mood-altering substances or compulsive behaviours. It creates a fast track into addiction and all the negative consequences that result from addiction.
This brings us to the final stage of the Vortex of Addiction: Oblivion. End-stage addiction is self-destruction, loss of control, loss of self, suicidal thoughts and actions, substance-induced psychosis, and all the profound impacts on health, relationships, and overall functioning.
The end stage of addiction is Oblivion.
Oblivion
Out of control. Rock-bottom. Skid-row. Oblivion. Some of the many words we use to describe the end of the road in addiction.
Oblivion is the outcome that results from chronic numbing and shutting down.
Rather than being able to heal and recover, a person continues to engage in unhealthy mood-altering ways of managing the overwhelming aspects of their lives. They are disconnected from healthy relationships and resources that provide support through the painful parts of life.
Although “oblivion” isn’t a clinical term in addiction treatment, it’s a good description of the detachment someone feels when addiction has taken over their lives. It reflects the experience of being disconnected from self, others, the future, and even reality. “Oblivion” includes such things as:
Chronic addiction
Severe negative consequences
Impacts on health
Homelessness
Mental health challenges
Withdrawal seizures
Substance-induced psychosis
Suicidal thoughts or behaviours
The loss of self that comes with addiction
What happens when people attempt to shut down and disconnect from the overwhelming and painful symptoms of unresolved trauma with mood-altering substances or compulsive behaviours? It creates a fast track into addiction and all of the adverse outcomes that come with addiction.
When a person has moved into this stage of the model, they often require significant intervention and support to help them move back into increased functioning. Without intervention, the consequences can be devastating.
Understandably, people want to shut down painful experiences and emotions – but it comes at a high cost. There is an enormous downside to addictive patterns of mood-altering.
In this stage, someone is far-removed from their “true self”. As a result, they experience such damaging consequences.
Loss of a Sense of Self
Addiction brings an almost total loss of willpower – the person cannot control their use despite their intentions. This loss of control with patterns of substance use becomes a chronic pattern, even though there may be a strong desire to stop.
A person in active addiction no longer has a choice: they must use their drug of choice to function.
One of the reasons for this is that individuals who use substances like alcohol, opiates, or benzodiazepines daily become physically dependent. As a result, they will experience severe negative physical or psychological symptoms when they stop using their substance. In some cases, this withdrawal can be life-threatening as it is with alcohol.
People lose their connection to their "true selves" when they are in addiction. Who they are is defined by the out-of-control patterns of addiction. As a result, countless broken promises are made to one's self and others.
Addiction makes people engage in behaviours they never thought they would do.
Important aspects of life get neglected – relationships, family, career, physical health, and finances all suffer. Values and morals get compromised. High-risk sexual behaviours occur. Laws get broken. Children are mistreated or neglected. No one sets out to do these things - this is the heartbreak of addiction.
The consequences of untreated addictive behaviour can be devastating across most aspects of a person’s life. Besides the obvious losses mentioned, some losses diminish a person’s sense of who they are. Essential parts of self like confidence, self-esteem, motivation, hopes, and dreams become more elusive.
Addictive substances and behaviours have a profoundly negative impact on how the brain functions. Impaired thought processes, decreased cognitive abilities, loss of concentration and changes in personality are some ways addiction changes how the brain operates.
Emotional Costs
Mood-altering decreases the ability to feel – it’s one of the “benefits” of substance use. But here’s the problem: while mood-altering diminishes the ability to experience painful emotions, it also alters the ability to feel good with the help of a substance. Long-term substance use also creates increased anxiety for many. More hostility, anger, and resentment can be directed towards anyone trying to confront the patterns of addiction, which leaves close relationships in turmoil.
Many of those in addiction use substances to avoid feeling bad rather than using them to feel “good”.
One emotion common among those in addiction is shame – that searing sense of failure that makes someone want to withdraw and hide. Shame tends to increase as the impacts of addiction increase. When life is impacted by addiction and the negative consequences of using, people are more likely to feel overwhelming shame. This overwhelming shame triggers the desire to continue mood-altering, creating a vicious cycle of shame and using addictive behaviours to numb it.
Physical Health is Compromised
The long-term use of drugs or alcohol can bring a severe deterioration in physical health. It creates an increased risk of malnutrition and other health consequences such as infections, liver disease, cardiovascular disease, and substance-related brain damage.
Alcohol addiction also brings significant health risks in the withdrawal process. For example, delirium tremens (DTs) is a severe form of alcohol withdrawal that includes tremors, agitation, increased heart rate, and even hallucinations. For someone addicted to alcohol, abruptly stopping the use of alcohol may trigger alcohol withdrawal seizures or create other life-threatening health consequences.
Mental Illness is Common
Chronic substance use and engagement in behavioural addictions have a profound impact on mental health. Although some people initially begin using substances to manage anxiety or depression symptoms, the process of addiction tends to increase mental health issues and leads to far more significant symptoms of anxiety, panic, depression, hopelessness, and suicidal behaviour.
One dramatic example of oblivion is the substance-related psychosis some users from experience from cannabis, cocaine, or methamphetamines.
Although suicide is often primarily considered a "mental health issue", suicide and suicidal behaviour are highly related to addiction disorders. We also know that trauma and PTSD increase the risk of suicidal ideation and suicide attempts. Addiction to drugs and alcohol increases the risk of suicide tenfold.
Suicide rates among polydrug users (using more than one substance) are up to 17 times higher than suicide rates in the general population.
Increased Risk of Additional Trauma
There are many sources of trauma in addiction. Even though some might view these negative consequences as "choices" made by a person, they are no less impactful because they come from addiction. These other overwhelming experiences can include:
Falls, injuries, and accidents
Serious health issues caused by substance abuse
Significant losses and negative consequences
Increased risk of violence or sexual trauma
Toxic impacts of substance use
Overdoses
Psychosis
Seizures
We are in the midst of an opioid overdose crisis in North America. Accidental overdoses have increased dramatically with the fentanyl crisis. There also is an alarming rate of deaths related to combining substances like alcohol and prescription drugs. In addition, polysubstance use has increased. Multiple substances lead to more unintentional ODs and more significant health and mental health problems.
Traumatic experiences endured in active addiction increase the trauma load, which, in turn, increases the mood-altering to manage trauma symptoms.
When a person has moved into this stage of the model, they often require significant intervention and support to help them move back into increased functioning. Without intervention, the consequences can be devastating.
Summing It Up
When someone in addiction reaches Oblivion, they often cannot break the addictive process alone. Therefore, they will usually remain there until they receive some intervention. They will need some form of help, such as medical support, addiction treatment, joining a recovery program, or seeking out therapy.
It is essential to reach out for support. The possibility of hope and recovery does exist.
The Vortex of Trauma & Addiction is a model that identifies how trauma and stress overwhelm us. If we don't find the resources to help us recover, mood-altering often becomes a way of coping – but serves to disconnect us from the things that assist in the recovery process.
I hope this model has given you a new way of looking at the process of addiction. As an addiction therapist, one of my beliefs is that "the problem is the problem". Addictive patterns of substance use and mood-altering are often a symptom of unresolved trauma or chronic stress rather than just the "problem".
It is essential to find a qualified therapist to help you address both addiction issues and the overwhelming life experiences that have created the desire to numb and disconnect.
Trauma-informed care recognizes the principles of safety and compassion are foundational to the process of healing and recovery for anyone experiencing a substance use disorder, especially when trauma has been a contributing factor.
I appreciate your interest in "The Vortex Model of Addiction” - it doesn't just speak to the journey into addiction. It also speaks to the process of recovery and the journey of healing. I am grateful to have an opportunity to do my part in bringing more compassion and more science to the field of addiction recovery.
Check out Recovery Happens
Carrie DeJong’s informative course that provides insight into the connection between trauma and addiction. It also explores pathways for healing and recovery.
References
(1) Office of the Surgeon General: Addiction and Substance Misuse Reports and Publications https://www.hhs.gov/surgeongeneral/reports-and-publications/addiction-and-substance-misuse/index.html
(2) Recovery Research Institute https://www.recoveryanswers.org/research-post/1-in-10-americans-report-having-resolved-a-significant-substance-use-problem/
(1) Khantzian, Edward J. "The Self-Medication Hypothesis Revisited: The Dually Diagnosed Patient." Primary Psychiatry Archive (2003). Primary Psychiatry. 2003.
(2) Felitti, Vincent J.; Anda, Robert F.; Nordenberg, Dale; Williamson, David F.; Spitz, Alison M.; Edwards, Valerie; Koss, Mary P.; Marks, James S. "Adverse Childhood Experiences". American Journal of Preventive Medicine. 14 (4): 245–258. (1998)
(3) Levine, Peter A. Waking the Tiger: Healing Trauma : The Innate Capacity to Transform Overwhelming Experiences. 1997.
(4) Van Der Kolk, Bessel. The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma. 2014.
(5) Porges, Stephen W. Clinical Application of the Polyvagal Theory. 2018
(6) Siegel, Daniel J. The Developing Mind. 1999
(7) Langeland, W., N. Draijer, and W. Van Den Brink. "Trauma and Dissociation in Treatment-seeking Alcoholics: Towards a Resolution of Inconsistent Findings." Comprehensive Psychiatry 43.3. 2002.